As new cases of the highly infectious Omicron variant continue to climb in undervaccinated parts of the world, we speak to the head of the Africa Centers for Disease Control and Prevention about how vaccine inequity could lead to even more variants of the coronavirus. Dr. John Nkengasong says only 10% of the population is fully immunized in Africa, a continent of 1.3 billion people, and millions of vaccines donated by COVAX went unused because of their short shelf life. Meanwhile, several countries in Africa have begun manufacturing their own vaccines. “We have to shift our focus to vaccinating — that is, making sure that vaccines that are arriving at the airport actually get into the arm of the people,” says Dr. Nkengasong.
TRANSCRIPT
This is a rush transcript. Copy may not be in its final form.
AMY GOODMAN: Global health leaders are warning that new cases of the highly infectious Omicron variant continue to climb in undervaccinated parts of the world. Only about 62% of the world’s population has received at least one shot, and the divide between the rich and poor regions remains vast. This is World Health Organization Emergencies Director Mike Ryan speaking virtually at the World Economic Forum last week.
DR. MICHAEL RYAN: If we look at in Africa, in our African regional office states, only 7%. So the reality is that the world is moving towards a 70% goal; the problem is we are leaving huge swathes of the world behind.
AMY GOODMAN: The World Health Organization says the wide vaccine gap could set the stage for another dangerous variant to emerge. This comes as top African health officials say nearly 3 million vaccine doses have expired on the continent. They say many of the doses donated by COVAX in individual countries had short shelf lives and arrived with short notice.
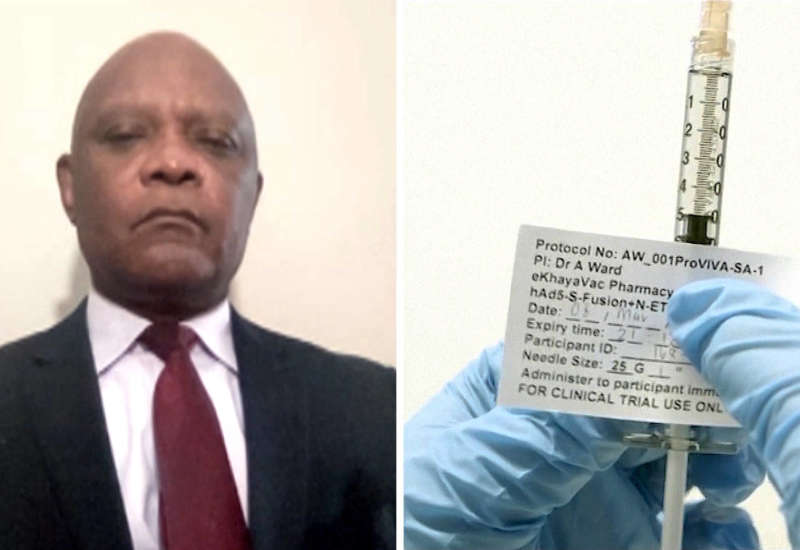
For more, we’re joined by Dr. John Nkengasong, director of the Africa Centers for Disease Control and Prevention, an institution of the African Union. He just wrote an op-ed in The New York Times headlined “There Will Be Another Variant. Here’s What the World Can Do Now.” He last joined us from Addis Ababa. Today he’s in Washington, D.C.
Dr. Nkengasong, welcome back to Democracy Now! So, talk about the state of the world right now, and particularly the African continent, when it comes to coronavirus. And what can be done now?
DR. JOHN NKENGASONG: Well, thank you for having me again on the program.
2022 must be the year that we completely tip the balance in favor of increased vaccinations in the developing world, especially in Africa. As we speak, just about 10% of the population in Africa, a continent of 1.3 billion people, have been fully immunized. I think we have a gap and a journey to get to the 70% target which the WHO has established. This is the year we must vaccinate at scale and at speed, if we have to defeat the emergence of new variants. We saw what Omicron did. Omicron taught us a lesson that any threat anywhere in the world is a threat everywhere in the world. So we really have to scale up vaccination using all the assets that we have and in a more deliberate manner, with stronger partnerships and collaboration across the board.
JUAN GONZÁLEZ: And, Dr. Nkengasong, from the issues of accessibility to the testing infrastructure and vaccine equity, why do these continue to be some of the most pressing demands that we face, especially in areas like Africa?
DR. JOHN NKENGASONG: So, the first challenge the continent had was access to vaccines. If you recall, the continent last year had very limited access to vaccines, including the AstraZeneca doses that were bought by the COVAX mechanism, but because of the ban that India posed on it, the continent was left with very limited vaccines. Now we are beginning to see a shift in that narrative, where more vaccines are arriving in the continent from COVAX, from the African Vaccine Acquisition Task Team, from bilateral donations like those offered by the United States government, which the continent is very appreciative.
But we have to shift our focus now to vaccinating — that is, making sure vaccines that arrive at the airport actually get into the arm of the people. Eighty percent of the population in Africa — 80% average — are willing to accept vaccines. There’s a 20% minority that are hesitant, but we can work on that. But let’s build the right alliances, partnerships, to get the 80% of the population that is keen to be vaccinated vaccinated. That is the only way we are going to save everyone everywhere in the world at the same time.
JUAN GONZÁLEZ: Now, you also wrote in an op-ed piece for The New York Times recently that was headlined “There Will Be Another Variant. Here’s What the World Can Do Now.” What are some of the steps that need to be taken now, because, as you say, inevitably, there will be more variants?
DR. JOHN NKENGASONG: There are a couple of things that the world must do, and do that collectively, not sequentially. One is to scale up vaccination. We’ve discussed that. Second is to test. We need to make sure that we have — we decentralize testing and make sure that the communities lead and own testing.
Thirdly, we need to increase our ability to monitor for these variants so that as they emerge, we know what exactly they are, what their properties are, and then take action, and, of course, make sure that that is linked to access to new drugs. We have new regimens that are out there, like the Paxlovid and other drugs. We should make sure that they are accessible so that when people are tested and they are positive, they get linked to treatment centers.
And lastly, let’s not let down our guards on the prevention measures. The prevention measures against — that we’ve used all through this pandemic — wearing of masks, avoiding large gatherings — work against all variants. Those must be maintained. Those are the key things that we need to do in 2022, and do all of it collectively.
AMY GOODMAN: I wanted to ask you about Moderna’s chair and co-founder, Noubar Afeyan, who was asked about patents by CNN’s Fareed Zakaria in an interview last month.
FAREED ZAKARIA: Let me ask you about this. A lot of people, or some people, are saying you guys should be giving this technology away, waiving all your intellectual patents. Explain what Moderna’s position on this is. As I understand it, you are willing to say you will not enforce patents as long as COVID is around.
NOUBAR AFEYAN: Well, Fareed, the first time we spoke was around the time a year ago when we voluntarily pledged — the only company to have done that — voluntarily pledged not to enforce our patents against anybody who uses our patents to make a vaccine against the pandemic. At that time, there had been no proof that the vaccine will work, but we did that because we thought it’s the right thing to do from a vaccine access standpoint. We believe that that has enabled others to make mRNA vaccines. And if others do that even further, that’s great.
AMY GOODMAN: So, that’s Moderna’s chair and co-founder. But, Dr. Nkengasong, there’s a difference between not suing a company for taking their recipe and revealing what that recipe, that formula is so that companies around the world could manufacture it and make it available, on the continent of Africa, in Asia, throughout the world. You have written and spoke about this at the World Economic Forum last week, when you said that during the pandemic we’ve seen a shameful collapse of global solidarity and cooperation. Can you talk about what these companies, that have made billions of dollars, paid for, in the research for them, in the case of Moderna, by U.S. taxpayers — Pfizer, because of its profits — paid for by the people, but not sharing these formulas? What effect has this had?
DR. JOHN NKENGASONG: So, this is a — we are living in an unprecedented time and dealing with a crisis that we’ve not witnessed for the last close to a hundred years. So that means the solidarity, that I’ve always been a champion of, has to be in play, solidarity that says that we need to bring all assets to the table to enable or increase availability or access of vaccines, including transfer of technology and also rights, and support for countries and regions to be able to manufacture vaccines, so that the issue of limited access to vaccines is overcome.
We are very encouraged that countries like the United States have already taken a position that favors that. We hope other developed countries will do the same. I’m also very encouraged that about 10 countries in Africa have now embarked on the journey of producing vaccines in their respective countries. Countries like South Africa, Rwanda, Senegal, Morocco, Egypt have all taken on their responsibility to produce vaccines in Africa. And that is very welcome, and they should be supported.
JUAN GONZÁLEZ: And, Doctor, I wanted to ask you, this whole issue of the number of shots that would protect one from COVID. We’re now seeing in countries like Israel now recommending a second booster. We’re talking about four shots in a period of about a year. It’s not really logistically possible for the world to keep up this kind of a vaccination program. What is your sense of what needs to be done by the manufacturers of vaccines in the future?
DR. JOHN NKENGASONG: Again, it goes back to the discussion we just had a few seconds ago, which is increased access to vaccines, and hopefully that the new generation vaccines will actually enable us to have the need to have the second, third and fourth dose less, I think.
But the issue we have in our hands right now is: How do we even get people that are struggling to get one shot to get that one shot? And how do we push or enable people that have received their only one shot to get their two shots, in Africa? I think the problem needs to be contextualized, so that we know exactly that you just cannot be aiming at the third and the fourth shot in Africa, where you don’t even have access to the first shot of the vaccine. So I think that is key. We should focus on vaccinating at scale, vaccinating at speed, especially in areas where there are limited vaccinations.
AMY GOODMAN: What do you know of a variant coming out of Cameroon that has also affected France, Doctor?
DR. JOHN NKENGASONG: We have had very limited information on that variant, and we have not seen any published data on that. And we hope — truly remain hopeful — that that is truly not a variant of concern.
AMY GOODMAN: And can you also talk about the expired vaccines, what it means when you get millions of vaccines in Africa? And really, let’s look at those numbers. You have NPR reporting that you have much of the midsection of Africa, including powerful economic and political players like Kenya, Nigeria and Senegal, all under 2% vaccination rates. Away from Africa, you’ve got 10%. People haven’t gotten about 10% COVID vaccine coverage, like Syria, Afghanistan, Haiti.
DR. JOHN NKENGASONG: Yeah. Any vaccine that expires is very painful, because that is potentially a life saved. But we should go beyond that and say, “What are the reasons that vaccines are expiring in Africa?” The first major reason is that those vaccines arrive with a very short lifespan, which is what you call the expiring date. So we have issued some guidance to any donations that the vaccines that are intended to be shipped to the continent should have at least a longer expiring date, at least three months to six months, so that the countries can prepare to use the vaccines then. Overall, about 0.5% of all vaccines that have arrived on the continent have expired. But again, I want to be very sure that I’m clear on this: Any expired vaccines that are on the continent is painful, because that is potentially a life that could be saved.
JUAN GONZÁLEZ: And could you talk about what some of the countries in Africa have gotten right in their efforts to prevent the spread of COVID, especially given the experience some had coping with the Ebola epidemics in the past?
DR. JOHN NKENGASONG: The continent has used several previous experiences in fighting the COVID pandemic, including mobilizing the community. I mean, at the Africa CDC, we’ve deployed over 18,000 community healthcare workers in several countries that do door-to-door engagement, human contacts, counseling and spreading of — helping the contact tracing early on in the pandemic.
The second thing the continent has done very, very well is really their cooperation. They’ve set up mechanisms like the African Vaccine Acquisition Task Team, which is a great symbol of intercontinental cooperation and collaboration, which has enabled the continent to secure over 450 million doses of vaccines. That is remarkable. It is the first time in the history of a disease that a continent has come together that much, under the very strong political leadership of President Cyril Ramaphosa when he was chair of the African Union.
So, such experiences must be maintained and must be operationalized and institutionalized, so that we can use such instruments to fight other pandemics in the future, and also to fight the existing endemic diseases. Let’s not forget that malaria, tuberculosis and HIV are still very serious health threats in Africa.
AMY GOODMAN: Yes, let’s follow up on that. Dr. Nkengasong, you’re not only the director of the Africa Centers for Disease Control and Prevention, but you are also nominated by President Biden for ambassador-at-large and coordinator of the U.S. government activities to combat AIDS/HIV globally. If you can talk about how the pandemic has affected these other diseases and populations dealing with, for example, TB, HIV/AIDS, etc.?
DR. JOHN NKENGASONG: Well, thank you. I’m truly grateful to President Biden for the nomination, but it still has to be confirmed. So, once that confirmation occurs, I’ll be at ease to speak more about the HIV pandemic.
But let me say just, very broadly, say that the disruption that COVID has had on the continent and impacted other diseases is huge. I mean, there’s no doubt about that. We have evidence from the Global Fund that clearly shows that services geared towards malaria, tuberculosis and HIV have been severely disrupted. So, I think that is what pandemics do. When you restrain people from moving, when you restrain and disrupt supply chain management, the overall impact is that there is a lot of severe impact on non-COVID-related affections.
JUAN GONZÁLEZ: And I wanted to ask you — during the pandemic, wealthier nations, like the United Kingdom, have relied on African doctors and nurses to shore up their health services. You’re calling on many of these doctors and nurses and health workers to return to Africa. Could you talk about this issue of the brain drain and of the — basically, the use of medical people trained in other countries by the wealthier nations?
DR. JOHN NKENGASONG: Absolutely. We learned a huge lesson during this pandemic, where we set up the African Task Force for COVID response, which is an intercontinental task force that coordinates the response and report to the level of the heads of states. And it was very interesting that so many Africans in the diaspora were willing to contribute — and contributed significantly — to the different technical working groups that were set up within this task force.
So, that suggested to us that if the African Union and Africa CDC would set up a deliberate program that will enable Africans who are in the diaspora to contribute their skill sets and experiences on the continent, it will be a remarkable return on investment. And that will enable them to at least help the continent, that has very limited human resources for health, to actually use that and address the challenges that we have. So we are looking into that very, very seriously.
AMY GOODMAN: Dr. Nkengasong, we want to thank you very much for being with us. You’re usually in Africa, born in Cameroon, but you’re in Washington, D.C., right now. What do you find, coming to the United States, the difference in how the people of the United States are dealing with, their attitudes toward, how the government is dealing with Omicron — but, overall, coronavirus — and the African continent?
DR. JOHN NKENGASONG: I think we have to admit that the Omicron variant is truly a lesson that this is a very difficult pandemic. It’s a difficult virus we’re dealing with. It’s a virus that mutates very quickly. It’s a virus that if you allow it to circulate, it’s going to create mutations and challenge even the vaccination efforts that we’ve had in the world.
I think we are very encouraged to see the leadership role that the United States is playing in making vaccines accessible to Africa. The United States has donated the most vaccines now in Africa. And the continent — I can speak on behalf of the African Union — is extremely grateful for that. So, that increased solidarity and leadership expressed by the United States in solving this problem globally is really going to be needed, going forward.
AMY GOODMAN: We want to thank you for being with us, Dr. John Nkengasong, founding director of the Africa Centers for Disease Control and Prevention, an institution of the African Union, recently nominated by President Biden for ambassador-at-large and coordinator of the U.S. government activities to combat AIDS/HIV globally. If confirmed, he would be the first person of African origin to hold the post. We will link to the New York Times op-ed that Dr. Nkengasong wrote, headlined “There Will Be Another Variant. Here’s What the World Can Do Now.”
Coming up, we will look at both the January 6th House committee and federal prosecutors, what they’re finding when it comes to the Capitol insurrection, and how that relates to a fascinating new book, Gangsters of Capitalism: Smedley Butler, the Marines, and the Making and Breaking of America’s Empire. Stay with us.